Search
Sharing Knowledge improves Knowledge... Knowledge should come at as less cost as possible.
Posts
Showing posts from May, 2014
Posted by
Varun C N
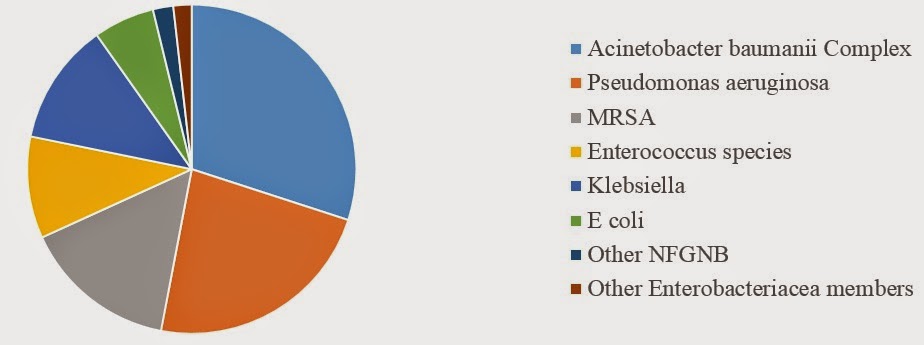
Health care associated Infection- basics
- Get link
- X
- Other Apps
Posted by
Varun C N
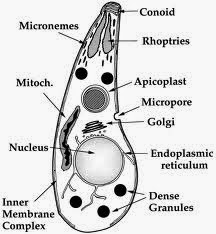
Does Toxoplasma drive you crazy?
- Get link
- X
- Other Apps

Posted by
Varun C N
Combo Therapy for TB
- Get link
- X
- Other Apps