Search
Sharing Knowledge improves Knowledge... Knowledge should come at as less cost as possible.
Posts
Showing posts from 2017

Posted by
Varun C N
Nobel Awards- 2017
- Get link
- X
- Other Apps

Posted by
Varun C N
Which viruses maybe seen in human semen
- Get link
- X
- Other Apps

Posted by
Varun C N
Zika Virus- Update III
- Get link
- X
- Other Apps

Posted by
Varun C N
Compound isolated from C difficile act against C difficile: Avidocin-CDs
- Get link
- X
- Other Apps

Posted by
Varun C N
Hypervirulent Klebsiella pneumoniae
- Get link
- X
- Other Apps

Posted by
Varun C N
Gonococcus superbug: Current Status
- Get link
- X
- Other Apps
Posted by
Varun C N
Scientists find a quick method to get Monoclonal Antibodies of interest.
- Get link
- X
- Other Apps

Posted by
Varun C N
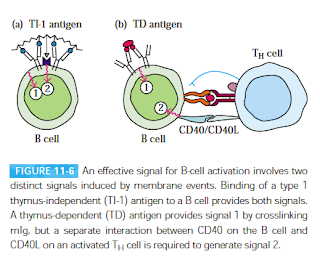
Dopamine says "Make antibodies"
- Get link
- X
- Other Apps

Posted by
Varun C N
nCD64 as a marker of Sepsis
- Get link
- X
- Other Apps
Posted by
Varun C N
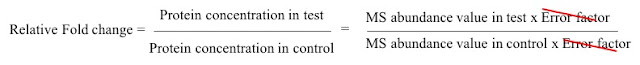
Lab series #17: Labelling methods for Quantitative Proteomics by MS
- Get link
- X
- Other Apps
