Some bacteria loves antibiotic
Greetings
That makes a sufficient introduction to the problem we are looking for. This is by far the greatest and strongest mode of bacterial resistance that we can expect to encounter. These strains are called as "antibiotic dependent bacteria". In a study published in Lancet, it was seen that, after the initial clinical treatment failure, the bacteria (in this case Enterococcus faecalis) was resistant to vancomycin but also needed it for its growth. Eltringham, a clinical microbiologist said "This is the first instance of isolating [the drug-dependent enterocci] in sick patients, where [the bugs] were almost certainly contributing to the infection" For reference and more details go here. Am not sure of what was the first report ever, but upon a literature search (Data digging!!!), I found an article by Dean JL etal to be the first reported case (Link).
The photo to the right shows a VDE (vancomycin dependent Enterococci). The VDE strain can only grow contiguous to the end of the strip with the highest concentrations. These strains are very difficult to deal with especially in Hospital settings. Reference
That leaves me thinking. How beneficial is that for the organism. The scenario is most probably something like this. The Clinician begins with an emperic antibiotic coverage till there is Microbiology report. Meanwhile the organism is mutating and acquiring resistance. When there is a report, the "right antibiotics" are given. Now the selection pressure enhances the resistance and an occasional mutant that can not only survive, but can actually utilize the drug, has now a competitive advantage and is selected. The clinician is now presented with a treatment failure, a grave one.
In a recent post (Link), I had summarized a few facts about the Antibiotic resistance problem. I also made an attempt to given an overview of various factors that can be involved in antibiotic resistance. So far so good. As a sequel to that post i will talk a little bit about antibiotic dependent bacteria.
Just to get head start, Antibiotics are substances (Primarily biological compounds), that can inhibit the growth or kill a cell. Sop, when we say antibacterial substances (Such as Penicillins, Carbapenems etc) we refer to an antibiotic that is acting against the bacteria. Simple. The best scenario (to us, not bacteria) is that the antibiotic acts against the bacterial providing clinical relief. But more often than not, the bacteria is not responding to many antibiotics. We say, its resistant. But now imagine what happens if the bacteria starts enjoying the antibiotics you are throwing at it, to an extent that the bacteria is now dependent on the antibacterial substance for its growth!!!
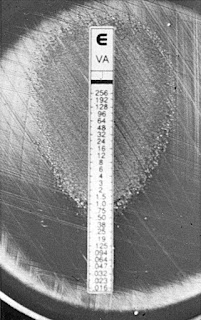 |
Photo 1: Vancomycin-dependent
enterococci (VDE)
|
The photo to the right shows a VDE (vancomycin dependent Enterococci). The VDE strain can only grow contiguous to the end of the strip with the highest concentrations. These strains are very difficult to deal with especially in Hospital settings. Reference
That leaves me thinking. How beneficial is that for the organism. The scenario is most probably something like this. The Clinician begins with an emperic antibiotic coverage till there is Microbiology report. Meanwhile the organism is mutating and acquiring resistance. When there is a report, the "right antibiotics" are given. Now the selection pressure enhances the resistance and an occasional mutant that can not only survive, but can actually utilize the drug, has now a competitive advantage and is selected. The clinician is now presented with a treatment failure, a grave one.
But then there is a second angle to this drama. The new "superbug" is now leaking to the community or to say a second person, the chances that it will survive is bleak. This is simply because the drug is now an obligation for growth. So unless and until the receiver is on that drug the organism is now selecting for mutants or just doesn't survive. That explains the fact that why this phenomenon is so rare.
After this incident, here and there a few cases of "Antibiotic dependent superbug" was seen. But then a big blow to this story came, when the phenomenon was reported for a tubercle bacilli. This time it is Tubercle strain dependent on Rifampin. The bacterium was identified in a patient in China, by researchers at the Johns Hopkins Bloomberg School of Public Health.
Once the organism develops a dependence, the implication of growing it in laboratory is serious. The strain may grow poorly and will be identified only when an enhanced growth is seen in the areas near to the drug. This is much more difficult when it comes to MDR-TB which is often difficult to grow. As Ying Zhang puts it "Rifampin-dependent tuberculosis is an unrecognized and potentially serious treatment issue. Rifampin resistance is ominous. Our study highlights the potential dangers of continued treatment of MDR-TB with rifamycins that occur frequently due to delayed or absent drug susceptibility testing in the field. Further studies are urgently needed to determine how common such rifampin-dependent MDR-TB is in field conditions and if it contributes to the worsening of the disease in MDR patients and treatment failures". Source
Perhaps such cases are under-reported and rare. But then, these are the strains that are the true superbugs.
Farrag N, Eltringham I, & Liddy H (1996). Vancomycin-dependent Enterococcus faecalis. Lancet, 348 (9041), 1581-2 PMID: 8950890
Tambyah PA, Marx JA, & Maki DG (2004). Nosocomial infection with vancomycin-dependent enterococci. Emerging infectious diseases, 10 (7), 1277-81 PMID: 15324549
Zhong M, Zhang X, Wang Y, Zhang C, Chen G, Hu P, Li M, Zhu B, Zhang W, & Zhang Y (2010). An interesting case of rifampicin-dependent/-enhanced multidrug-resistant tuberculosis. The international journal of tuberculosis and lung disease : the official journal of the International Union against Tuberculosis and Lung Disease, 14 (1), 40-4 PMID: 20003693



Comments
Post a Comment