BtB#4- Sterilization/Disinfection in brief
Greetings,
A huge number of medical procedures especially surgical relies heavily on the use of safe and sterile equipment. Most of the consumables, especially in molecular biology and microbiology requires that they are sterile and devoid of any organisms, to avoid external variables in the experiment. "Microbial sterilization" is a very serious concept. Failure to comply with standard protocols have lead to problems. Probably the shipment of live anthrax (failing inactivation) to several research laboratories, is one of the latest and most commonly cited examples. There are several methods to choose from, and not every method can be used on every type of material. In some cases, you don't need high degree of sterility and some cases you do. This post, will deal with some basic concepts in brief rather than a very in depth talk.
Coming to definitions, Sterilization has been defined as "Sterilization describes a process that destroys or eliminates all forms of microbial life and is carried out in health-care facilities by physical or chemical methods". In contrast, Disinfection is defined as "a process that eliminates many or all pathogenic microorganisms, except
bacterial spores". There are scenario's where though sterility would be ideal, all that is possible is disinfection. For example, during blood collection for culture, you cannot sterilize the skin where venipuncture is to be made. You can however, disinfect.
 |
| Fig 1: Sterilization/Disinfection methods. Source |
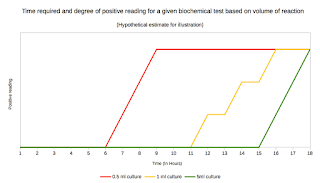
There are several methods of sterilization and disinfection. They are very broadly classified into physical and chemical methods. Fig 1, shows a typical textbook classification of the methods. It has been broadly accepted of all the methods autoclave, a method of moist heat sterilization is the best possible method when available. But here is an important catch. Sterilization by any of the methods listed is not 100% fool proof. The efficiency of sterilization depends on the microbial load. The lower the load, better sterilization.
Let me explain. The measurement of sterilization is SAL (Sterility assurance level). SAL is defined as the probability of a single unit being non-sterile after it has been subjected to sterilization. Let us take an example. Say you have a 100 ml nutrient broth to be sterilized. It is not possible to make a 100% accurate prediction that every possible organism has been destroyed in the broth after sterilization. Rather, you could calculate a probability of the chances. For all practical purposes, sterilization is considered as good enough if you achieve a six-log reduction in numbers. That means if you started with 106 organisms, there is a still a possibility that one organism is potentially viable, yet sterilization is declared as complete. So hence if you start with a very dirty equipment, without even a prior cleaning (such as simple washing which will remove a large amount of microbes), sterilization will be grossly incomplete.
There are several bodies that scientifically evaluate methods and recommend the standards to be followed. For most part, especially microbiology practices used standards set by The European Committee for Standardization (CEN), which develops sterilization standards through CEN/TC 204, Sterilization of Medical Devices. Other bodies include The International Organization for Standardization (ISO) and The Association for the Advancement of Medical Instrumentation (AAMI). All 3 standards have similar requirements though have minor differences.
 |
| Table 1: Risk Classification |
As I have already stated, not all materials that are used needs a very high level of sterility. To determine the requirement, materials are classified into 3 classes. See Table 1. Detailed guidelines and explanation of work procedures can be found from CDC page here. A serious drawback of almost all the methods already described is the viability of prions. Though it is not a common scenario to encounter prions, these agents extremely difficult to be inactivated. They are stable at very high temperatures and also are resistant to strong chemicals. If prion contamination is suspected, autoclaving for 1 hour or a method called "Gas Plasma Sterilization" method is considered efficient.
 |
Photo 1: Components of a Self-Contained
Rapid Readout Biological Indicator.
|
Controlling for sterilization is a hot topic. Traditional methods used Physical and chemical indicators. Biological indicators (BIs) are most reliable and commonly used. Earlier technologies used strips containing spores. These days a more directly readable BIs are in use. For example, a sealed ampule containing spores of Geobacillus steraothermophilus coated onto a strip is embedded. This ampule also contains a crushable second glass ampule. After sterilization process, the glass ampule is crushed allowing medium to flow. If the spores are alive the organism will grow producing a color change in the medium.
A very detailed notes about sterilization and disinfection is given here. For notes on testing of chemicals for their sterilization/disinfection capabilities see here.


Comments
Post a Comment