Health care associated Infection- basics
Greetings
I have been recently brushing through some literature on hospital acquired infections. Needless to say, this is a matter of global concern. I have absolutely no intention of talking about the common organisms involved, but want to highlight certain basics which I believe needs a blog space.
There are several definition that you would find on Nosocomial infections. For a reference let us consider the WHO definition. “Health care associated Infection (HCAI)” can be defined as an infection acquired in hospital by a patient who was admitted for a reason other than that infection. An infection occurring in a patient in a hospital or other health care facility in whom the infection was not present or incubating at the time of admission. This includes infections acquired in the hospital but appearing after discharge, and also occupational infections among staff of the facility.
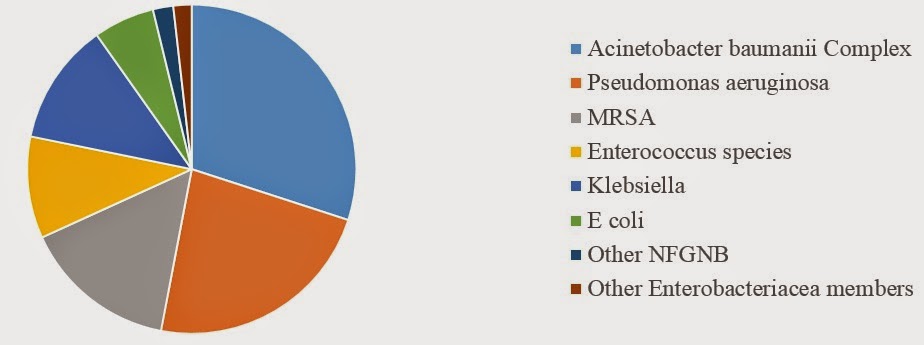 |
| Fig 1: Commonly encountered bacterial pathogens in HCAI. |
If you search literature on HCAI, you had see a lot of papers dealing with bacterial isolates. Irrespective of the place where the data is generated you had see the 5 organisms appearing in the important list- Acinetobacter species, Pseudomonas aeruginosa, MRSA, Enterococcus species and Klebsiella pneumoniae. If I had construct a chart of the common bacterial isolates it had look something like the one shown in Fig 1. Of these Pseudomonas aeruginosa and Acinetobacter baumanii complex, are extra ordinarily regular in showing up in culture plates. If your thinking where did the star pathogen C difficile go, I'm coming to that point of discussion in the later part.
My first question is why Acinetobacter, Pseudomonas and MRSA are always the star Trio? The answer lies in their viability and isolation rate. It is wrong to claim that they are the common bacteria seen in the hospital. They represent a very fast growing organism in the culture plate and are viable in environment even in extreme conditions. Pseudomonas for example is one of the hardest pathogen that can be thought of. It can survive significant amount of disinfectants that are thrown on in it including phenol to an extent. That's exactly why we use Phenol agar (I used to call it Dettol agar!!!), for specific isolation. Second, they grow in the least of nutrients and easily isolated in the clinical laboratory. Hence reported. If I had consider viruses, parasites and fungus then there are much less reports available. My understanding is that Candida and Aspergillus species are more common among the fungus. Of them non albicans candida is significant.
What causes HCAI? In the pre antiseptic era, the hospital infections where much high in number often being fatal. With introduction of Anti septic techniques this have reduced. But the single most important thing among them is Hand-washing. As more recent papers indicate, there is still less than 40% compliance in health care workers. This is the most important factor even to this day. Solution to the problem exists such as use of Hand-rubs but much less of it is practised than said.
A question that I once thought of was "Shouldn't it be that only organisms originating from health care set up be included in hospital acquired infections?". Let me elaborate. If a patient is put on a urinary catheter, and the patient acquires E coli- UTI, should it be called Hospital acquired. The organism came from the patient himself. The answer is still "Yes". It doesn't matter where did the organism actually come from. The essence is "If its a product of medical intervention?".
Despite a century old history of Nosocomial infections, there is a little data on the dynamic of these infections. The first step to study the actual dynamics of such a complicated system involving multiple variables is to know what the hospital actually harbours. This requires an extensive analysis. A simple petri dish culture involves only a few organisms. Modern third generation sequencers have enabled us to look into much more depth. In other words, "Hospital Microbiome" is the data we are now looking for. There currently is a project going on (Link), with some preliminary data.
There has been some studies trying to get the hospital system more resistant to harbouring pathogens. One of the most well known approach include use of bacteriophage solutions that maybe sprayed on surfaces. The approach though fascinating, is not a long time viable approach. More recently the concept of use of copper surfaces in the hospital has shown promise.
What causes HCAI? In the pre antiseptic era, the hospital infections where much high in number often being fatal. With introduction of Anti septic techniques this have reduced. But the single most important thing among them is Hand-washing. As more recent papers indicate, there is still less than 40% compliance in health care workers. This is the most important factor even to this day. Solution to the problem exists such as use of Hand-rubs but much less of it is practised than said.
A question that I once thought of was "Shouldn't it be that only organisms originating from health care set up be included in hospital acquired infections?". Let me elaborate. If a patient is put on a urinary catheter, and the patient acquires E coli- UTI, should it be called Hospital acquired. The organism came from the patient himself. The answer is still "Yes". It doesn't matter where did the organism actually come from. The essence is "If its a product of medical intervention?".
Despite a century old history of Nosocomial infections, there is a little data on the dynamic of these infections. The first step to study the actual dynamics of such a complicated system involving multiple variables is to know what the hospital actually harbours. This requires an extensive analysis. A simple petri dish culture involves only a few organisms. Modern third generation sequencers have enabled us to look into much more depth. In other words, "Hospital Microbiome" is the data we are now looking for. There currently is a project going on (Link), with some preliminary data.
There has been some studies trying to get the hospital system more resistant to harbouring pathogens. One of the most well known approach include use of bacteriophage solutions that maybe sprayed on surfaces. The approach though fascinating, is not a long time viable approach. More recently the concept of use of copper surfaces in the hospital has shown promise.
In short, hospital acquired infections represent a standard problem of modern day health care system. The problem is currently addressed by frequent surveillance, constant vigilance of Infection control committee and safe medical practices. However, it is also true that hospital is a microbial heaven.
Smith, Daniel. (2013-04-15) The Hospital Microbiome Project: Meeting Report for the 1st Hospital Microbiome Project Workshop on sampling design and building science measurements, Chicago, USA, June 7th-8th 2012. , 8(1), 112-117. DOI: 10.4056/sigs.3717348
Allegranzi B, Bagheri Nejad S, Combescure C, Graafmans W, Attar H, Donaldson L, & Pittet D (2011). Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet, 377 (9761), 228-41 PMID: 21146207



.svg.png)
Comments
Post a Comment