Rapid tests for Ebola
Greetings
One of the first tests to have brought in the hope was RPA (Recombinase Polymerase Amplification) method, a technology developed by TwistDx Ltd. The entire diagnostic kit could be packed into a suit case, operated by an integrated solar panel and a power pack. Famously dubbed as Diagnostics-in-a-Suitcase, results can be produced in 15 min. The technique is an Isothermal amplification method. Isothermal amplification makes use of polymerase that can both make and break DNA strands without having to cycle between temperatures. In RPA a Staphylococcal Sau polymerase does the work. By combining it with probes that can fluoresce upon amplification the reaction can be carried in a rapid and reliable way. One of the other famous Isothermal amplification method include- LAMP assay.
The second test that has an increasing importance is a immunology based detection method. The test uses standard immunochromatography method, something similar to the pregnancy test kit. The test known as ReEBOV Antigen Rapid Test Kit has been approved under rapid approval protocol by WHO. the test correctly identifies 92% of infected people and 85% of uninfected ones. Most of the immunology based tests were sensitive enough but not as good as molecular. This is of course expected, since the molecular can pick up even the slightest trace. However, rapid tests allow for screening which is important in removing those people from the scene who are not likely to be positive. Cary Gunn, chief executive of Genalyte comments on use of raid tests, “There’s a great deal of interest in a technology that can screen large numbers of people from a finger prick in only a few minutes, you can imagine testing an entire planeload of passengers and screening through them cost-effectively.”
More recently a silver nanoparticle based lateral flow test has been developed. Use of nanoparticles in diagnostic is fairly a recent concept and has been well researched upon in multiple context. For example Silver particles have been used in a technique called Au-nanoprobe hybridisation, which can be used for SNP detection. That is just an example. An entire range of tests including genomics, proteomics, MEF (Metal enhanced Fluorescence) methods have been developed based on silver nanoparticles. In a new method published in Lab on a chip, The test strip contains a paper strip with antibodies attached to silver nanoparticles of varying sizes. These nanoparticles have a property that they will produce different colors when presented in different sizes. When patients serum sample diffuses via lateral flow antibody attached silver particles flow along producing a distinctive color line which can be visualized. The test has been optimized to detect Yellow fever, Ebola and dengue. The strip measuring around 8×3 cm takes 10 minutes at a cost of 2$ per test. This is one of the finest examples of next generation Laboratory detection technology.
It would be interesting to see and compare the efficiency of these rapid tests in field and how well could they contribute to the control of current Ebola outbreak. Even if the performance is slightly low these tests have great potential as a screening toolkit.
 |
| Fig 1: Distribution of Ebola cases. |
The Ebola 2014 outbreak that began in March 2014, has been one of the toughest outbreak that is successfully restrained by an international effort. As of on 11 Feb 2015, a total of 22894 cases have been reported with 9177 deaths (case fatality ratio= 40.08%). Fig 1 shows the distribution of cases in intensely affected regions. A total of 65 new confirmed cases were reported in Guinea, 3 in Liberia, and 76 in Sierra Leone in early February. A very detailed data on the current situation has been reported by the WHO (Link). The statistics looks quite impressive in comparison with the numbers during the active outbreak. However, new cases are a worry and efforts are on to pin it down. Th last traces of cases are really hard to wipe out in any outbreak.
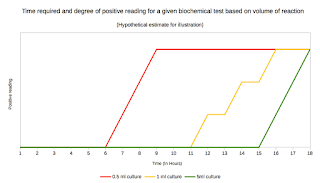
The complete control of EBOV outbreak will be possible with rapid diagnosis and effective measures post diagnosis. I have already talked about Ebola vaccination and treatment strategies under evaluation in my previous posts. Routine diagnostics by PCR or other molecular methods require its own time, which is a significant window to the problem (Link). Point of care testing have been an attractive candidate for development.
 |
| Photo 1: Diagnostics-in-a-suitcase. Source |
 |
| Photo 2: ReEBOV Kit. Source |
 |
| Photo 3: Nanoparticle based Lab chip Source |
It would be interesting to see and compare the efficiency of these rapid tests in field and how well could they contribute to the control of current Ebola outbreak. Even if the performance is slightly low these tests have great potential as a screening toolkit.
Vogel G (2014). Infectious Diseases. Testing new Ebola tests. Science (New York, N.Y.), 345 (6204), 1549-50 PMID: 25258059
Yen CW, de Puig H, Tam JO, Gómez-Márquez J, Bosch I, Hamad-Schifferli K, & Gehrke L (2015). Multicolored silver nanoparticles for multiplexed disease diagnostics: distinguishing dengue, yellow fever, and Ebola viruses. Lab on a chip PMID: 25672590
Larguinho M, & Baptista PV (2012). Gold and silver nanoparticles for clinical diagnostics - From genomics to proteomics. Journal of proteomics, 75 (10), 2811-23 PMID: 22119545
Larguinho M, & Baptista PV (2012). Gold and silver nanoparticles for clinical diagnostics - From genomics to proteomics. Journal of proteomics, 75 (10), 2811-23 PMID: 22119545



Comments
Post a Comment