The link between Brain and Microbiome
Greetings
I had previously blogged on significance of microbiome in brain health. Though the exact mechanisms are under investigation, several studies have pointed that this is not a mere correlation. Psychiatric conditions such as schizophrenia are heavily investigated with reference to oral and gut microbiome. It has been proposed that altering the microbiome may be beneficial in influencing the brain health, which is the basic concept of psychobiotic's.
 |
Fig 1: C. albicans IgG levels and seropositivity
in schizophrenia and bipolar disorder
compared to controls. Source
|
However, I would also like to think of the following possibility. At least a subset of patients with psychiatric illness has lower hygiene. And it is well known that improper hygiene can lead to candida infection. The paper also finds that C albicans exposure was associated with homelessness in bipolar males. That makes my suspicion higher. 26% correlation according to me is far less of an evidence warranting a significant look. I perhaps would want to see this paper in a different angle. People with Schizophrenia or Bipolar disorder needs to be screened and promptly treated for Candida infections.
I want to present a totally different example linking brain chemistry and microbe. In a recent proof of principle study in mouse models, it has been shown that LPS from bacteria can target TLR4 - a receptor which is also present on the surface of gut cells, taste cells and immune cells, which influences sweet receptor genes in taste buds, reducing sweet cravings. Administering LPS to mice also blocked leptin receptors. In other words, bacterial contents can have an effect on something as fundamental as food craving behavior.
 |
Fig 2: Comparison of Proliferation, Survival and Neurogenis in Conventionally
colonized, Germ free and germ-free–colonized mice. Source
|
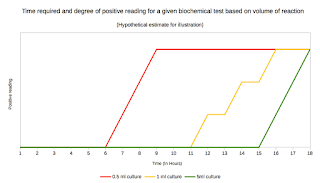
I presented a couple of case examples here from recent papers to illustrate that microbes have something to do with Brain chemistry but not necessarily all correlation studies indicate that there is a direct connection. But the question remains as to if there is a real connection at least in a few cases. The answer is yes. Several studies have reported that there is a connection between adult hippocampal neurogenesis and gut microbiome. In a study published in 2014 by Ogbonnaya et al, 10-week-old mice were injected with bromo- deoxyuridine (BrdU) to label proliferating cells and euthanized 2 hours later. The neuronal sprouting was measured between a normal and germ-free mice. They found that Germ-free and germ-free–colonized mice exhibit a trend for increased cell proliferation as measured by bromodeoxyuridine immunohistochemistry. The study also found that postweaning microbial colonization of germ-free mice did not prevent changes in adult hippocampal neurogenesis, which suggested that there is a critical window in early life during which microbial colonization influences adult hippocampal neurogenesis.
 |
| Table 1: Organisms influencing on Neurotransmitter activity. |
It has been the understanding from different studies that Neurotransmitters production can be influenced by microbes. Some examples are shown in Table 1. In a study by Bravo etal, it had shown that L. rhamnosus (JB-1) induced region-dependent alterations in GABAB1b mRNA in the brain in a mouse model. In another study by Tillisch et al, fermented milk product probiotic (FMPP) was administered for 4 weeks to healthy women. The study found alterations in intrinsic activity of resting brain indicated that ingestion of FMPP was associated with changes in midbrain connectivity. Such studies stands as a proof that indeed administering the right microbe can contribute in treating Brain health.
 |
| Table 2: Psychobiotic studies. Source |
Now that I have made a clear argument that microbial influence on brain chemistry is indeed a reality as I have previously argued I want to introduce the concept of Psyhchobiotics. Psychobiotic is defined as a cocktail of live organism that, when ingested in adequate amounts, produces a health benefit in patients suffering from psychiatric illness. Studies from like that mentioned above and many other indicate that psychobiotic can be the future of psychiatric treatment. We are yet to find the right combination of organisms. As shown in Table 2 which summarizes published Psychobiotic studies several possibilities and leads are already proposed.
There are several explanations of how a microbiome can connect with the neural system and influence the behavior. This includes communication through gut-brain axis, production of metabolites or chemicals that influence Neurotransmitters or modulate receptor activity etc. Now a new study has proposed a totally new concept- influencing through immune cells. The study proposes a specific subset of immune cells- Ly6Chi Monocytes can function as a possible mediator between gut, immune cells and neurons. The researchers here studied Antibiotic treated adult C57BL/6 mice to investigate the impact of gut flora dysbiosis on hippocampal neurogenesis.
 |
| Fig 3: Classification of Monocytes. |
Before I get into the details, let us first clarify what is Ly6Chi Monocyte. As everyone knows, monocytes are large phagocytic white blood cell with a simple oval nucleus and clear, greyish cytoplasm. They can further differentiate into macrophages or dendritic cells. Each of these cells can be identified using flow cytometry analysis. Traditionally monocytes are classified into 3 types. See Fig 3 for details. Each type is further sub typable based on the markers displayed on the cell. I mean to emphasise that monocytes are not a homogenous population. The circulating monocyte population is divisible into Ly6c positive monocytes and Ly6c negative monocytes. Both types express CD115 and CD11b. In a flow cytometry run, we can identify two populations of blood monocytes: Ly6c+ monocytes (CD11b+ CD115+ Ly6Chi) and Ly6c− monocytes (CD11b+ CD115+ Ly6c−). Neutrophils also express Ly6C but can be distinguished since monocytes express higher levels of Ly6c than neutrophils. That's why Ly6Chi is an important feature here. Interestingly, Ly6c+ monocytes are precursors of Ly6c− monocytes. By the way, Ly6C stands for lymphocyte antigen 6 complex. Macrophage and dendritic cell precursors in the bone marrow give rise to Ly6Chi monocytes, which serves as an intermediate for Ly6Clow monocyte generation. Here the superscript hi or low stands for expression of the marker Ly6C. Ly6Chi monocytes exit the bone marrow in a CC-chemokine receptor 2 (CCR2)-dependent manner and are recruited to inflamed tissues. So functionally, Ly6Chi monocytes are inflammatory monocytes selectively traffic to the sites of inflammation.
In the current study, researchers administered mice antibiotics to free intestine from microbes. When compared with untreated mice, the mice who lost their healthy gut bacteria performed low in memory tests and showed a loss of neurogenesis in hippocampus. They also noted reduced Ly6Chi monocytes in brain, blood, and bone marrow. Further experiments showed that reduction in levels was correlated with loss of neurogenesis and this could be rescued by replenishing the Ly6Chi levels.
 |
| Table 3: Contents of VSL#3 Probiotic mixture. |
Subsequent experiments showed that though probiotics helped the mice regain memory, fecal transplants to restore a healthy gut bacteria did not have an effect. The probiotic used in this study was VSL#3, which is a mixture of eight different strains of bacteria. VSL#3 works by colonizing the GI tract and forms a barrier that protects the inner layer of the gut from pathogens. VSL#3 positively affects a variety of substances that are involved in gut function. This is important to ensure the correct absorption of nutrients and to maintain barrier function. The VSL#3 contents are shown in Table 3.
 |
| Fig 4: Impact of prolonged antibiotic treatment on brain cell plasticity and cognitive function. Source |
In conclusion, Psychobiotics appears to be a real thing and microbial community does have important function in regulating Brain health. I guess, there will come a day when psychiatric treatment regimen will also include giving specific cocktail of organisms to improve patient symptoms. Who said bacteria are all bad.
Severance, E., Gressitt, K., Stallings, C., Katsafanas, E., Schweinfurth, L., Savage, C., Adamos, M., Sweeney, K., Origoni, A., Khushalani, S., Leweke, F., Dickerson, F., & Yolken, R. (2016). Candida albicans exposures, sex specificity and cognitive deficits in schizophrenia and bipolar disorder npj Schizophrenia, 2 DOI: 10.1038/npjschz.2016.18
Ogbonnaya ES, Clarke G, Shanahan F, Dinan TG, Cryan JF, & O'Leary OF (2015). Adult Hippocampal Neurogenesis Is Regulated by the Microbiome. Biological psychiatry, 78 (4) PMID: 25700599
Möhle, L., Mattei, D., Heimesaat, M., Bereswill, S., Fischer, A., Alutis, M., French, T., Hambardzumyan, D., Matzinger, P., Dunay, I., & Wolf, S. (2016). Ly6Chi Monocytes Provide a Link between Antibiotic-Induced Changes in Gut Microbiota and Adult Hippocampal Neurogenesis Cell Reports DOI: 10.1016/j.celrep.2016.04.074



Comments
Post a Comment