Isolated Immunology inside Central Nervous system
Greetings
This blog has focussed quite a lot on the concepts of core microbiology. As an occasional drift, today I want to talk about a topic that is one of the fields with very less literature available on hand. Don't get me wrong. Am not going to talk about extreme geeky stuff, but just the basics. A rare field of Microbiology, Neuro-Microbiology and its counterpart, Neuro-Immunology. So here's a question for you to gaze at. The popular view that used to exist in the field of medicine is "Neuro" is a Immunoprivileged site. If thats the case, someone once asked "How the antibodies and cellular Immune response to Neural infections if there is very little exchange and immunologically inert?"
The popular scientific view was that CNS (Central nervous system), is a highly protected area and there is a very little exchange of molecules (very tightly regulated exchange) from the other parts of the body compared to CNS. In reality, this holds true for many molecules. The molecules found in the CSF (Cerebrospinal fluid), which baths the CNS is in equilibrium with serum molecules. The ratio of molecules (generally) in CSF being approximately, 1/3rd of that in serum. Of course there are exceptions.
This blog has focussed quite a lot on the concepts of core microbiology. As an occasional drift, today I want to talk about a topic that is one of the fields with very less literature available on hand. Don't get me wrong. Am not going to talk about extreme geeky stuff, but just the basics. A rare field of Microbiology, Neuro-Microbiology and its counterpart, Neuro-Immunology. So here's a question for you to gaze at. The popular view that used to exist in the field of medicine is "Neuro" is a Immunoprivileged site. If thats the case, someone once asked "How the antibodies and cellular Immune response to Neural infections if there is very little exchange and immunologically inert?"
The popular scientific view was that CNS (Central nervous system), is a highly protected area and there is a very little exchange of molecules (very tightly regulated exchange) from the other parts of the body compared to CNS. In reality, this holds true for many molecules. The molecules found in the CSF (Cerebrospinal fluid), which baths the CNS is in equilibrium with serum molecules. The ratio of molecules (generally) in CSF being approximately, 1/3rd of that in serum. Of course there are exceptions.
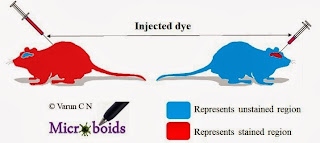 |
| Fig 1: Experiment demonstrating the BBB |
In 1880's Paul Ehrlich experimentally observed, intravenous administration of dyes stained all organs except the brain and the spinal cord. In 1913, Edwin Goldman, demonstrated the same dye when directly injected into the CSF, readily stained nervous tissue but not other tissues. The experiments for the first time indicated that there was a barrier that separated the two anatomical regions. However, it was Lewandowsky, while studying potassium ferrocyannide penetration into the brain, was the first to coin the term blood-brain barrier. Later experiments used basic lipid soluble dyes, which could stain all parts including CNS, showed that there was a direct transport of the dyes across the cerebral microvasculature. Further studies by Broman concluded that it was not a single system. The barrier is a two component system, Blood-CSF barrier (BCB) at the choroid plexus and the blood-brain barrier (BBB) at the cerebral microvasculature. The final confirmation came from EM studies by Reese and his team demonstrating the barrier to the capillary endothelial cells within the brain by electron-microscopic studies. For source and more details, refer here.
 |
| Fig 2: The BBB and BCB. Source |
The BBB and BCB maintain the cellular and chemical contents of CSF within strict limits. Lipid soluble substances within blood can diffuse across. However, passages of fluids, ionic and polar substances requires facilitated transport. Na+ an important component nerve firing, is transported via passive diffusion and Na-K pump. Potassium is however, actively removed from CSF circulation. Interesting to note that the substances as important as glucose, amino acids, certain hormones (such as insulin) requires specialized transport. Chloride (Cl) represents a major anion in the CSF, and its concentration is 15-20 mEq/L higher than in serum. Earlier papers suggested that in Tubercular meningitis (TBM), Cl concentration was lowered and the test was used to predict TBM. This was thought to be due to a breach in BBB. However, we now know that it is simply a reflection of lower serum values. What I mean to say is CSF chloride levels is no more considered a diagnostic or prognostic marker for TBM. The Acid- Base balance is also maintained by the choroid plexus. It can remove weak organic acid and antibiotics such as Penicillins, cephalosporins, aminoglycosides from CSF.
Give this some thought. CNS is THE MOST important part to protected. Theoretically speaking, we should have had an immune system, that is more aggressively active in this part. But the truth is, it isn't. I understand given the importance, to have a specialized gate mode of entry but why immunologically less active? The restriction of movement is so much that even molecules such as IgM is not allowed to cross. There is vritually no lymph node (Although Virchow Robin space is considered as a analogus version of Lymph node of brain). The possible answer is, Immunity is a double edged sword. The battleground of immunity often leads to damage to neighbouring cells, through inflammation, a risk that cannot be taken easily in the nerve environment. Maybe thats why we have evolved our CNS to be preferentially previleged.
The concept of Neuro-inflammation is quite complex. When warranted (physiological and pathological) the CNS can respond to a variety of factors, such as pathogens, toxins, degeneration etc. Surprisngly the neuronal activity can itself activate the immune system of immunity. A recent publication, suggests the term "Neurogenic Neuroinflammation" for inflammatory reactions in the CNS in response to neuronal activity.
Digressing from the above, I will put forth a question. Is autoimmunity bad? Conventional scientific wisdom is "Of course bad". Autoimmunity is not always pathogenic. A certain degree of autoimmunity is required to Destroy abnormal, dead cells, Tumor immunity and the more recent researched field- "Protective autoimmunity", which pertains to role of Neuro-inflammation for repairs in CNS. I have put forward this idea here just to illustrate it to you one of the lead roles of tight regulation of immune cells, that is served by the selective barriers of CNS. That should hint you a connection between Neurogenic Neuroinflammation and Protective autoimmunity
Let me put the whole thing in a perspective. Yes, Neuro-immunology is a total different way of operating of immune cells in context to CNS. There is a special barrier that possibly excludes a large subset of leucocytes from accessing the brain microenvironment. However, certain subset of cells can involve in the CNS immunosurveillance. In other words, CNS controls its own immunosurveillance (by selectively regulating cell trafficking), a luxury not available at any other part of the body. The immune functioning (Inside the CNS) plays significant role in supporting normal stem/progenitor cell renewal and neurogenesis, hippocampal-dependent cognitive ability and attention, and they are crucial for containing mental stress by enabling its resolution, and for fighting off depression. Reference
Give this some thought. CNS is THE MOST important part to protected. Theoretically speaking, we should have had an immune system, that is more aggressively active in this part. But the truth is, it isn't. I understand given the importance, to have a specialized gate mode of entry but why immunologically less active? The restriction of movement is so much that even molecules such as IgM is not allowed to cross. There is vritually no lymph node (Although Virchow Robin space is considered as a analogus version of Lymph node of brain). The possible answer is, Immunity is a double edged sword. The battleground of immunity often leads to damage to neighbouring cells, through inflammation, a risk that cannot be taken easily in the nerve environment. Maybe thats why we have evolved our CNS to be preferentially previleged.
The concept of Neuro-inflammation is quite complex. When warranted (physiological and pathological) the CNS can respond to a variety of factors, such as pathogens, toxins, degeneration etc. Surprisngly the neuronal activity can itself activate the immune system of immunity. A recent publication, suggests the term "Neurogenic Neuroinflammation" for inflammatory reactions in the CNS in response to neuronal activity.
Digressing from the above, I will put forth a question. Is autoimmunity bad? Conventional scientific wisdom is "Of course bad". Autoimmunity is not always pathogenic. A certain degree of autoimmunity is required to Destroy abnormal, dead cells, Tumor immunity and the more recent researched field- "Protective autoimmunity", which pertains to role of Neuro-inflammation for repairs in CNS. I have put forward this idea here just to illustrate it to you one of the lead roles of tight regulation of immune cells, that is served by the selective barriers of CNS. That should hint you a connection between Neurogenic Neuroinflammation and Protective autoimmunity
Let me put the whole thing in a perspective. Yes, Neuro-immunology is a total different way of operating of immune cells in context to CNS. There is a special barrier that possibly excludes a large subset of leucocytes from accessing the brain microenvironment. However, certain subset of cells can involve in the CNS immunosurveillance. In other words, CNS controls its own immunosurveillance (by selectively regulating cell trafficking), a luxury not available at any other part of the body. The immune functioning (Inside the CNS) plays significant role in supporting normal stem/progenitor cell renewal and neurogenesis, hippocampal-dependent cognitive ability and attention, and they are crucial for containing mental stress by enabling its resolution, and for fighting off depression. Reference
Abbott NJ, Rönnbäck L, & Hansson E (2006). Astrocyte-endothelial interactions at the blood-brain barrier. Nature reviews. Neuroscience, 7 (1), 41-53 PMID: 16371949
Xanthos DN, & Sandkühler J (2013). Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nature reviews. Neuroscience PMID: 24281245



Comments
Post a Comment