Make in India: Rotavirus Vaccine
Greetings,
Gastro-intestinal infections represent one of the most common group of infections, especially so developing countries. Hygiene is the most contributing factor with paediatric population at highest risk. As per the statistics Rotavirus is the leading cause of severe diarrhoea in children in developed and developing countries. The Statistics from Indian scenario is not very good but the estimates are that approximately 1.5 lakh children die from rotavirus infection in India each year. The launching of indigenously developed Rotavirus vaccine recently has been welcomed by many. Here is some basic details on Rotavirus and vaccine program.
 |
| Fig 1: Rotavirus replication. Source |
Rotavirus (Reoviridae family) was first identified in 1973 as a viral etiological agent of diarrhoea. Structurally it resembles a wheel-shaped virus. Its genome consists of 11 double-stranded RNA segments coding for six structural proteins (VP1, VP2, VP3, VP4, VP6 & VP7) and six nonstructural proteins (NSP1-6). Virion spike containing VP4 is proteolytically cleaved by intestinal proteolytic enzymes (Mainly trypsin) to yield VP5 and VP8. VP5 is primarily responsible for permeabilisation of cells to the virions. There are at least eight species of this virus, referred to as A, B, C, D, E, F, G and H. Among all of them Rotavirus A is responsible for more than 90% of rotavirus infections in humans.
Rotavirus is a completely preventable infection, since the neutralising antibodies against the spike proteins are effective. The very first vaccine that was tried against Rotavirus was introduced in 1998. This consisted of Bovine rotavirus strain NCDV (Nebraska Calf Diarrhoea Virus) which was renamed as RIT4237. Subsequently Rhesus rotavirus (RRV), and later a RRV reassorted with human rotavirus VP7 proteins with G-types G1, G2 and G4 was used which was called as RRV-TV (RRV- Tetravalent). This was marketed as RotaShield from 1998. It was then withdrawn, with the observation that it was associated with intussusception. Following these, several other vaccines have been tried and tested, as shown in Table 1. Of these RotaTeq and Rotarix has been licensed for commercial purposes.
 |
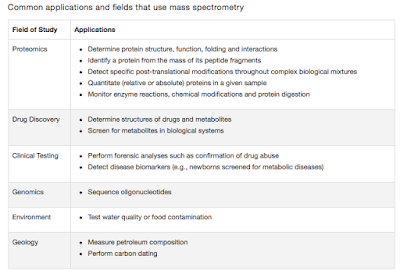
| Table 1: Rotavirus Vaccines. |
The pilot studies by Bharath Biotech was done on 2 strains- 1132 and 116E. According to the patent details filed, The human rotavirus strain 116E is a human-bovine reassortant with human G9 strain containing bovine VP4 gene homologous to the P[I l] gene segment. The 1321 strain is Gl OP [1 1], primarily composed of bovine genes and has only two gene segments of human origin, VP5 and VP7. The original 1 16E (G9[P11]) and 1321 (GlOP[I l]) were adapted to grow in cell culture by passages in primary African green monkey kidney (AGMK) cells then in MAl 04 cell substrate and later in serially Passaged AGMK (SPAGMK).
Rotavac consists of 116E strain prepared in Vero cells. Each dose of 0.5 mL contains NLT 105.0 FFU of live rotavirus 116E. As per the recommendations, the vaccine is to be administered as a 3-dose regimen, 4 weeks apart, beginning at 6 weeks of age and should not be administered to children older than 8 months of age. Based on a double blind study published in Lancet, the efficacy for severe non-vaccine rotavirus gastroenteritis was 56.4% in the first year of life and the vaccine efficacy in the second year of the same study was 49%. The findings was heavily debated since a near 50-60% efficiency is not really good. There are 2 ways of looking at it. Chandrakant Lahariya commented, “ In a disease like rotavirus-related diarrhoea with a huge burden it will indeed have a huge impact in terms of the number of lives saved. Interventions in all ways should be tried to save the maximum number of lives. The price of the vaccine at just about US$1 is also not so huge.” Jacob Puliyel comments, “It is a toss-up if the vaccine will work for you. If 100% [of the] population is vaccinated it will reduce 50% [of the] rotavirus deaths. What are the numbers needed to treat [to prevent one death]?”.
Despite the efficacy not being ideal, the vaccine has been licensed and launched for use earlier this month. Scientists have urged that more work is needed and there is scope for improvement. As Soumya Swaminathan, director general of ICMR states "It can certainly be better because 50-60% is not the ideal efficacy rate. And so there is research underway to improve efficacy because one of the observations that has been made is that the efficacy of oral vaccines is generally lower in India than it has been in developed countries -- the same had been observed with polio also. The exact reason is not known, but it could be related to the high rate of enteric infections (related to the intestines) that children here have. People are looking at various strategies to increase the efficacy of the vaccine and of course there are people who are looking at different vaccines also. So maybe in the future better vaccines may be available. But at this point in time, we have a good, cost-effective vaccine".
Bhandari N, Rongsen-Chandola T, Bavdekar A, John J, Antony K, Taneja S, Goyal N, Kawade A, Kang G, Rathore SS, Juvekar S, Muliyil J, Arya A, Shaikh H, Abraham V, Vrati S, Proschan M, Kohberger R, Thiry G, Glass R, Greenberg HB, Curlin G, Mohan K, Harshavardhan GV, Prasad S, Rao TS, Boslego J, Bhan MK, & India Rotavirus Vaccine Group (2014). Efficacy of a monovalent human-bovine (116E) rotavirus vaccine in Indian infants: a randomised, double-blind, placebo-controlled trial. Lancet, 383 (9935), 2136-43 PMID: 24629994




Comments
Post a Comment