BtB#8- Resistance, Persistence and Tolerance
Greetings,
It just so happened that I was talking about antibiotic resistance and the topic popped up about antibiotic resistance in terms of tolerance and persistence. Most commonly when an organism grows in the presence of a defined cutoff value of antibiotic concentration we just call it "Resistant". That's what we are measuring when performing an antibiotic susceptibility testing. But everything that doesn't kill is not resistance. Confused? As early as 1944, it was observed that bacteria were able to survive extensive antibiotic treatments without acquiring resistance mutations. To contrast with true resistance, these were termed as "Tolerant".
Antibiotic resistance is a topic I have talked about too many times in the blog and hence it is not worthy to spend time talking about it again (People interested please refer my earlier posts). These concepts are not well illustrated and sometimes terms like- "Persisters, Tolerant and Resistance" are used interchangeably.
 |
| Fig 1: Methods of phenotypic resistance. Source |
Let us clarify what each term means. Resistance refers to an inherent ability of microorganisms to grow at high concentrations of an antibiotic irrespective of the duration of treatment. This is quantified in the laboratory by measuring MIC. Tolerance is defined as the ability to survive transient exposure to high concentrations of an antibiotic without a change in the MIC. Persisters are not mutants but are rather phenotypic variants randomly produced in a population. They are simply non-growing dormant cells and overcome the antibiotic attack simply by being totally inactive (which essentially makes them un-targetable). Most of the literature agree that persisters are simply an extreme case of tolerance. Another term that is often used is drug indifference. The usage of this term is very inconsistent in literature. Drug indifference occurs when the antibiotic is effective only in a specific bacterial physiological condition. Resistance requires changes in genetic code. Tolerance and persistence don't.
If persistence is an extension of tolerance, then why different terminologies? The answer is, tolerance and resistance are a phenomenon of the whole population. In contrast, Persistence is a phenomenon of a subpopulation. Persistence is observed when most of the population is rapidly killed and a subpopulation residue still continues to just be there, even though genetically they are clones. Tolerance is achieved by slowing down some essential step that is targeted by antibiotic. The best example is β- lactam resistance by slowing down the cell wall assembly. Persistence can be achieved through staying in Lag phase for a very long time (Type I) or by halting the growth (Type II).
 |
| Fig 2: Characteristic drug responses of resistance, tolerance and persistence. Source |
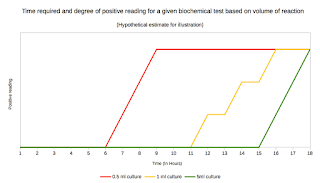
These properties can be differentiated by an assay called MDK (Minimum duration for killing). MDK is a measure of tolerance based on the idea that a tolerant strain requires long exposure time to be effectively killed than a susceptible strain. The MDK is defined as the typical duration of antibiotic treatment that is required to kill.
As can be seen from figure 2, MIC cannot distinguish between a resistance and tolerance, but MDK can. MIC for a tolerant strain of bacteria is similar to that of a susceptible strain; However, MDK is significantly higher for the tolerant strain. A persistent strain and susceptible strain of bacteria have a similar MIC and MDK99. However, the MDK99.9 is substantially higher for a persistent strain than the MDK99.99 of a susceptible strain. MDK99 means MDK for 99% of cells and MDK99.99 means MDK for 99.99% of cells.
An especially interesting case is the persistence through a gene called as hip. In E coli, hyperactivation of HipA through mutation leads to 100 to 1,000-fold increases in persistence. Basically, it generates two subpopulations with very different lag time distributions to one another. This can be identified using culture kinetic assay which will show a bimodal killing curve. There are many similar cases reported in the literature. A bacterial division is imperfect and except for the DNA, nothing is absolutely distributed between two daughter cells. This leads to different types of daughter cells sometimes with varying susceptibility to antibiotics. The best example of this case scenario is MTB. MTB divides asymmetrically and one of the two daughter cells will usually be longer and faster growing than its twin. In a recent study researchers from Tuft's university showed that these longer bacteria were least affected by rifampicin.
Most of us have an impression that antibiotic sensitivity has to do with genotype. This is not true always. Antibiotic sensitivity has also contextual dependence such as time of exposure and the state of bacteria. Most bacteria have a far from "Ideal bacterial growth curve". Most bacteria have a stringent control on what machinery is under operation and this can be regulated to advantage under antibiotic stress. One of the most effective mode is the stationary phase, which is especially resistant.
To conclude, resistance is not the only mechanism to resist antibiotics. You can tolerate it or persist over it.
Brauner A, Fridman O, Gefen O, Balaban N. Distinguishing between resistance, tolerance and persistence to antibiotic treatment. Nature Reviews Microbiology. 2016;14(5):320-330. doi:10.1038/nrmicro.2016.34
Corona FMartinez J. Phenotypic Resistance to Antibiotics. Antibiotics. 2013;2(2):237-255. doi:10.3390/antibiotics2020237
Kirill Richardson, Owen T. Bennion, Shumin Tan, Anh N. Hoang, Murat Cokol, Bree B. Aldridge. Temporal and intrinsic factors of rifampicin tolerance in mycobacteria. PNAS, 2016; 201600372 DOI: 10.1073/pnas.1600372113



.svg.png)
Comments
Post a Comment