Indigenously developed Leprosy vaccine
Greetings
Recent buzz of talk is revolving around the leprosy vaccine. An indigenously developed vaccine by G.P Talwar, (Founder-director of National Institute of Immunology) which uses a strain Mycobacterium indicus pranii (MIP). Let us look into some details.
 |
| Fig 1: Leprosy pathogenesis. Source |
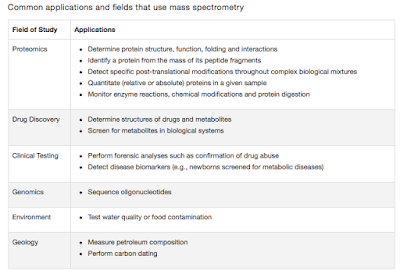
Leprosy is caused by M leprae, one of the least understood Mycobacterium species. The bacilli are acquired by inhalation though it is not clearly defined how do the bacilli reach back to the respiratory system and discharged. Another rare mode of transmission involves direct skin contact (Though not common such cases have been reported).
The bacilli basically infect the peripheral nervous system. Though the details are not clear, current evidence suggests that the bacilli attack Schwann cells. The immune system comes into play and cellular response (CD4+ T cell response) leads to granulomatous lesions and intense intraneural oedema. The subsequent destruction of schwann cells and axons leads to nerve function impairment, a hallmark feature of leprosy. Most often the diagnostic is quite straightforward with a deep skin smear. Clinically, five forms of leprosy are defined which includes lepromatous leprosy (LL), borderline lepromatous (BL), mid-borderline (BB), borderline tuberculoid (BT), and tuberculoid leprosy (TT).
WHO estimates the global prevalence of leprosy at about 0.24 cases per 10 000 people (Data doesn't include Europe). This is well within the WHO's aim of a prevalence rate of less than 1 case per 10000 persons. But, India stands out in global statistics of Leprosy. As per 2013-14 statistics, nearly 59% of new leprosy cases in the world are from India. 2013-14 alone registered 1.27 lakhs new cases in India.
When I searched the literature for Leprae vaccines, I find that people have tried a variety of stuff. This includes- BCG with killed M leprae, BCG with M vaccae etc. The first significant publication of GP Talwar regarding Leprae vaccine based on MIP has come in 2005. The study was a double-blind study and the vaccination schedule of the Healthy household contacts comprised two doses at 6-month intervals. The first dose of vaccine consisted of 1x109 autoclaved MIP bacilli in 0.1 ml physiological saline (0.85% NaCl), while the subsequent doses contained half the number of bacilli. The study showed an overall prophylactic efficacy of 65–70%. The idea that MIP could serve as a surrogate comes from a publication in 1991 showing that MIP shares numbers of common B and T cell determinants with M leprae.
 |
| Photo: GP Talwar. Source |
MIP (earlier known as Mw) is a cultivable, non-pathogenic and rapidly growing saprophyte classifiable in Runyon's group IV- Mycobacterium avium complex. Its use as an adjunct in TB therapy has been shown to be useful and studies are investigating its potential against TB cases.
Dr Soumya Swaminathan comments, "It is the first vaccine for leprosy, and India will be the first to have a large-scale vaccination programme. Trials have shown that if the vaccine is given to people in close contact with the affected, cases can be brought down by 60% in three years. It expedites cure rate if given to people with skin lesions".
Currently, a clinical trial is aimed to be started. About 7.5 crore people have been screened across the country (from 50 high-risk regions), of which 5000 have been confirmed with leprosy. The idea is to treat the diagnosed cases and prophylactically give rifampicin to close contacts. It is not clear to me about the vaccine trial design. But I think the idea would be to administer the vaccine in these high-risk areas and look for a reduction in number of cases.
Yadava A et al. T-Cell Responses to Fractionated Antigens of Mycobacterium w, a Candidate Anti-Leprosy Vaccine, in Leprosy Patients. Scand J Immunol. 1991;34(1):23-31.
Sharma et al. Immunoprophylactic effects of the anti-leprosy Mw vaccine in household contacts of leprosy patients: clinical field trials with a follow up of 8-10 years. Lepr Rev. 2005 Jun;76(2):127-43.
Gupta A et al. Efficacy of Mycobacterium indicus pranii Immunotherapy as an Adjunct to Chemotherapy for Tuberculosis and Underlying Immune Responses in the Lung. PLoS ONE. 2012;7(7):e39215.



Comments
Post a Comment