Antibiotic resistance- The basics
Greetings
Infectious diseases represent one of the most important paradox. Most of the infectious diseases in immuno-competent individuals is caused by a small set of pathogenic microbes. The treatment is well defined in these set of organisms. However, even with well defined set of protocol to treat an infectious agent, the clinical care takers find it incredibly difficult to treat the organism. In this post, I want to elaborate on the issue of antibiotic resistance in context with treating bacterial infections.
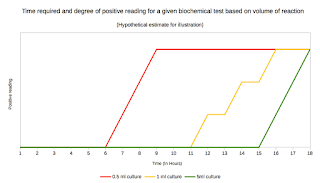
Antibiotic resistance can be classified into- Intrinsic and Acquired resistance. Intrinsic resistance refers to non responsiveness to an antibiotic (usually a Subclass of drug) due to lack of target, that has been acquired by the organism as a part of its species character. Each species of interest is intrinsically resistant to a group of antibiotics. The intrinsic resistance for an organism is well characterized for clinically relevant species. A prior knowledge of this resistance pattern is important when treating a given infectious condition on a case by case basis. The Intrinsic resistance, though hampers the choice of antibiotics, isn't a significant chunk of problem because it is a non changing phenomenon (Not always the case).
Acquired resistance represents, acquiring resistance to antibiotic through single or multiple changes that can be stably inherited from generation to generation. It can also be passed from one strain to another (or swapped in between genus). The patterns of resistance is not consistent at a global scale and the prevalent antibiogram has to be prepared locally. An antibiogram is a report that reflects the percentage of a given organism that is susceptible to each of the antimicrobial agents routinely tested.
 |
| Fig 1: Acquired resistance |
Its a common knowledge in clinical microbiology that the Gram negative infections are harder to treat, and highly resistance evolving type in comparison to Gram positive organisms. The question that is raised immediately is where does the resistance evolve from? The best explanation provided is natural selection. The normal mutation rate of the organism allows an occasional microbe to be generated that is resistant to the antibiotic. This population extends over a period of time replacing the original sensitive strain. Years of research and billions of dollars are pulled out to bring out an antibiotic. And the resistance is evolved, just like that (The sad part).
 |
| Fig 2: Resistome Source |
The second most common mode of antibiotic resistance is through gene transfer. Many different antibiotics are inspired from nature. The antibiotics in use today are naturally existing compounds that is found in nature for thousands of years (Probably even millions!!!). Resistant genes are thus circulating in gene pool that has evolved. The genes just need to be transferred. The entire set of gene pool in a given bacterial community that can mediate resistance is referred as Resistome. The largest set of resistome, is probably Soil Microbiota.
Understanding of mechanism of evolving resistance has some interesting set of implications. Irrespective of that the resistance is acquired through a mutation (slow ever evolving mechanism) or gene transfer (Rapid, leap in resistance) we can reverse the phenomenon, by removing the selective pressure. The genes are intact in a species and carried over for a long series of time over the generation only when there is a selective advantage of having it. That means, by the same mutation that brought in the resistance to an antibiotic, can also reverse it by another mutation. It can be stably inherited, if there is no selection pressure to keep the resistance gene. This is one of the central concepts of Antimicrobial Stewardship. Antimicrobial stewardship programs (ASPs) advocate for judicious use of available antimicrobials to preserve their usefulness.
 |
| Fig 3: Bystander effect. |
So far so good. But then, there is a third mode of antibiotic resistance that is not much discussed in the literature perhaps because of its undermined importance. This is called as Passive resistance or as i would like to call it more aptly, "Bystander Resistance". The idea is quite simple. Take this scenario. If there happens to be a sensitive organism in proximity to a resistant organism. Moreover the resistant bacteria secretes, an enzyme that mediates resistance, then the sensitive bacteria can benefit from bystander effect. I have explained this in Fig 3 to the left. For an argument on the bystander effect, go here. This phenomenon, though not convincing on the first look, is indeed shown to be true at least in one case. In Otitis media condition, Weimer etal; demonstrated that NTHi (nontypeable Haemophilus influenzae) provides passive protection for S. pneumoniae in vivo through production of β-lactamase.
That leads to a question someone asked me. If organism is in CNS and sensitive to a particular drug, but you cannot use it, because the antibiotic cannot penetrate the Blood-Brain-Barrier, then the resistance will be called as? (By the way, crossing BBB has to do with lipid solubility of the drug). According to me the question is baseless. This is a case where the bacteria enjoys the privilege of site, where the antibiotic cannot reach, rather than anything from the part of microbe. So its not resistance at all. I suppose that clarifies.
So I can summarize, there are 3 modes of bacterial resistance- Intrinsic, Acquired and Passive resistance. The resistance mechanism under each can be classified as follows
- Impermeability to the drug
- Absence of target site
- Lack of enzymes to convert the Pro drug to the active form
- Alteration in anti-microbial target
- Reduction or nullifying cell permeability to drug penetration
- Decreased uptake of antibiotic by expression of efflux pumps
- Production of an enzyme that inactivates the drug
- Production of an alternate pathway that bypass the action of drug
- Biofilm formation
Let me talk some basic ideas and concepts under each.
Changes in outer membrane permeability:
This was early recognized early in history of antibiotic development that natural penicillin was effective only against Gram positive organism but not against Gram negative bacteria which is attributed to the impermeability of the outer membrane. Mutations in specific porins, formation of biofilm and large size of the drug with respect to the channels of influx also contribute significantly to resistance mechanism.
Inner membrane impermeability:
Many drug molecules bind to a transporter molecule (E.g.: Anionic transporter in aminoglycoside) which subsequently is transported to the cytoplasm across the membrane by a proton motive force (PMF). The PMF that is required for substrate transport into the cell is often mutated in resistant strains. This generally is seen after a stepwise mutation in chromosome.
Promotion of antibiotic efflux:
The drugs that are used may not reach optimal intracellular concentrations which are due to active efflux the drug. The process is usually due to acquiring of a new protein that is plasmid encoded and hence easily transmitted. This mechanism is also possible owing to a chromosomal mutation which is well noted in 4 genes-PenA, PenB, PonA and mtrR that encode increased expression of an efflux pump. Such an active efflux system is well studied in E.coli against norfloxacin.
Alteration of target:
Resistance to various different antimicrobial agent is mediated this mechanism. The resistance is usually acquired through a single step or multistep mutation in chromosome or a plasmid that is expressive. The target may be modified in enzyme binding site (e.g.: Rifampicin resistance), Receptor mutation (e.g.: MRSA due to PB2’) or ribosomal targets (e.g.: Macrolide resistance). The change is mostly due to a chromosomal mutation or in some instances through recombination.
Bypass of antibiotic inhibition:
This mechanism though not common is of importance as it creates very stable auxotrophic mutants. The organism by mutation loses some gene activity which encoded for a protein that was a target for the drug. The new variant is unable to synthesize the compound and becomes dependent. This may affect virulence in a few scenarios.
The above described mechanism reflects a broad way of defining the resistance mechanisms that an organism is able to use in an unpredictable format. In any given organism multiple mechanisms may exist in co-existence can lead to pan-resistant (e.g.: Pan-drug resistant Acinetobacter, PDRA), multidrug resistant (e.g.: Multidrug resistant Enterococci, MDRE), extremely resistant (e.g.: Extremely drug resistant Mycobacterium tuberculosis, XDRTB) or super resistant types (e.g.: Super drug resistant Enterococci, SDRE).
Forsberg KJ, Reyes A, Wang B, Selleck EM, Sommer MO, & Dantas G (2012). The shared antibiotic resistome of soil bacteria and human pathogens. Science (New York, N.Y.), 337 (6098), 1107-11 PMID: 22936781.
Khadem TM, Dodds Ashley E, Wrobel MJ, & Brown J (2012). Antimicrobial stewardship: a matter of process or outcome? Pharmacotherapy, 32 (8), 688-706 PMID: 23307518.



Comments
Post a Comment