The Rise of Superbug Gonococcus
Greetings,
The world is talking about the emergence of MCR-1 and every single time a new strain is detected it is a news. Brazil recently reported its first case. A case was also reported from New Jersey of a strain that carried MCR-1 and NDM-5. I have already talked about MCR-1 gene multiple times and there is nothing new (except reporting of more new cases). MCR-1 has taken over so much of the news space that one another phenomenon is just not getting the right coverage. I intend to draw some attention on the increasingly reported resistance to antimicrobials by Gonococcus.
 |
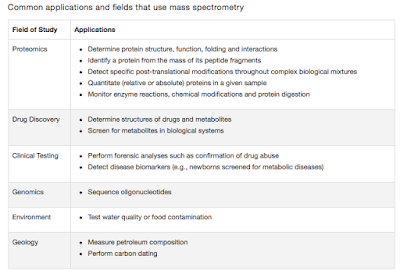
| Fig 1: Antibiotic resistance in Gonococcus. Source |
Gonococci is kind of special member in the Neisseria group by their ability to accumulate genes. Until early 1980's most of the strains were sensitive to penicillin. Resistance began emerging rapidly and by 2010, resistant strains have been circulating for most of the antibiotics in the panel. The last 2 antibiotics in the resort have been ceftriaxone and azithromycin. Over the period since, most strains have acquired resistance to azithromycin and all chemicals of quinolone class.
Quinolone resistance has some interesting consequences. Quinolones attack DNA gyrase and DNA topoisomerase which is essentially involved in keeping the DNA structure in right shape. It has been hypothesised that mutations in these which help overcome quinolone resistance indirectly can influence the mutation rate and thus increase resistance to other drugs. This has also shown to be the case in a couple of experiments though it has been heavily debated across the community. Whatever is the case, currently at least in the UK gonococcal resistance has reached a new peak and most are resistant to almost everything except for ceftriaxone. WHO has expressed its concern over the issue. With roughly 78 million new cases globally reported every year, a sudden superbug phenomenon is projected. WHO has released its new guidelines recommending complete elimination of quinolone from the treatment panel. This is the first recommendation change coming after 2003. There is a catch. Though WHO recommends cephalosporins, 46 countries have reported gonorrhoea strains with decreased susceptibility to ceftriaxone, and 10 have reported patients for whom none of the usual antibiotics was effective.
The following statements by Zenilman capture the whole story
The following statements by Zenilman capture the whole story
"Gonorrhea has been plaguing humanity for centuries. But ever since penicillin came along a dose of antibiotics would usually take care of the disease. Gonorrhea used to be susceptible to penicillin, ampicillin, tetracycline and doxycycline very commonly used drugs. But one by one, each of those antibiotics and almost every new one that has come along since eventually stopped working. One reason is that the bacterium that causes gonorrhoea can mutate quickly to defend itself. If this was a person, this person would be incredibly creative. The bug has an incredible ability to adapt and just develop new mechanisms of resisting the impact of these drugs."
 |
| Fig 2: Cases of highly azithromycin-resistant Neisseria gonorrhoeae 2014 to February 2016 in the UK. Source |
To have a look at how bad is the situation in the UK, I traced a literature describing Azithromycin resistance in gonorrhoea cases. Fig 2, summarised here is a clear layout of the problem. A strain can be called as High-level Azithromycin-resistant if MIC >256 mg/L. These strains also possess multiple genes for resistance and is widely resistant to almost every possible drug. They are sometimes referred in the literature as XDR-Gonococcus.
Kai Kupferschmidt wrote an interesting article in science, suggesting that there is a reasonably good possibility that gonococci are going to be soon resistant to all the antibiotics that can target the bacteria, and this will be the first true superbug.



Comments
Post a Comment