ETX2514: A new Beta Lactamase Inhibitor
Greetings
Antibiotic resistance is a scary topic to talk about. I have discussed in detail why we could never have an antibiotic for which resistance couldn't develop (Link). The emergence of MCR-1 colistin resistant gene is something that we really didn't want to see. Hospital-associated infection is a common topic discussed everywhere because a lot of hospitals is a place containing all the nasty drug resistant pathogens. There is a global movement to invent new antibiotics and there is political support in some countries to fast track development of new antibiotics. Currently new generation antibiotic is really needed against ESKAPE pathogens. In this group, the gram negatives are the first priority targets, with Acinetobacter topping the list, especially in a hospital setting.
 |
| Fig 1: Pipeline of Entasis Therapeutics. Source |
Entasis Therapeutics (AstraZeneca spinout) is one such company interested in developing antibiotics, has secured $50 million to progress its pipeline of drugs. It has announced the initiation of Phase 1 clinical study of ETX2514. The study will evaluate the safety, tolerability and pharmacokinetics of ETX2514 in healthy volunteers. The clinical trial will be conducted in Australia (124 volunteers) and is expected to be completed in the first half of 2017.
Robin Isaacs Chief Medical Officer of Entasis Therapeutics comments, “We are very enthusiastic about the initiation of this clinical study, which will begin to establish the safety, tolerability and administration profile of ETX2514 in the clinic. This study builds on our extensive research in preclinical infection models which indicate that the administration of sulbactam in combination with ETX2514 holds great promise against drug-resistant A baumannii infections." The company is also currently advancing an oral drug to treat gonorrhoea through mid-stage clinical trials. It is also involved in developing intravenous and oral drugs for pneumonia, blood infections, urinary tract infections, and infections following surgery, though those are all in preclinical stages of development.
Robin Isaacs Chief Medical Officer of Entasis Therapeutics comments, “We are very enthusiastic about the initiation of this clinical study, which will begin to establish the safety, tolerability and administration profile of ETX2514 in the clinic. This study builds on our extensive research in preclinical infection models which indicate that the administration of sulbactam in combination with ETX2514 holds great promise against drug-resistant A baumannii infections." The company is also currently advancing an oral drug to treat gonorrhoea through mid-stage clinical trials. It is also involved in developing intravenous and oral drugs for pneumonia, blood infections, urinary tract infections, and infections following surgery, though those are all in preclinical stages of development.
To digress, there are a few compounds that are in clinical testing against ESKAPE pathogens and many of them are yet to clinical trials. I found an interesting list of drug candidates that are currently in testing phase with possible potential.
 |
| Table 1: Some antibiotics against ESKAPE pathogens in Phase 3 testing. Source |
As I have mentioned several times in my previous posts (See my posts here, here and here), it is easier to invent something that will make the existing drugs sensitive rather than invent something that is totally new.
 |
| Fig 2: Structure of ETX2514. Source |
ETX2514 a β-lactamase inhibitor. Chemically, it is diazabicyclooctenone. Because it is potent against multiple classes of β-lactamase enzymes, ETX2514 expands the spectrum of gram-negative, drug-resistant bacteria. I couldn't find any formal publication about this drug and hence for digging the details am relying on a poster presented about the drug in Microbe 2016 ASM conference.
I gain from the details presented, the company first performed a whole genome sequencing of 132 A baumanii isolates and found a variety of resistance encoding bla genes (Molecular class A, C and D). There is a very small group of strains having molecular class B bla genes. Most of them possessed Class D. Class D is same as functional group 2d. They are poorly inhibited by clavulanic acid, "bla genes" are β-lactamase encoding genes. Thus it makes sense to attack these products. Based on structure-based design and quantum mechanics calculations series of diazabicyclooctenones was identified. ETX2514 is an improved chemistry design from the original design. Interestingly, ETX2514 covalently binds to the catalytic Ser-90 of AmpC and displays a similar conformation to avibactam. It can strongly bind to Penicillin-binding proteins (PBP).
 |
| Fig 3: Main conclusions of the presentation on ETX2514. Source |
The results from the study state as follows
"MIC90 of any BL combined with ETX2514 was ≤ 0.12 mg/L against both K pneumoniae and E coli. Imipenem was the most effective BL partner for ETX2514 against P aeruginosa (MIC90 = 2 mg/L) while sulbactam was the most potent partner against A baumannii (MIC90 = 4 mg/L)". Other conclusions from the study are shown in Fig 3.
It is true that sulbactam is used clinically as a β-lactamase inhibitor (BLI). It is known that the chemical also has inherent antibacterial activity against a few such as Neisseria gonorrhoeae, Bacteroides fragilis and Acinetobacter species, which works by binding through PBPs. Sulbactam inhibits PBP1 and PBP3 but not PBP2 in A baumannii.
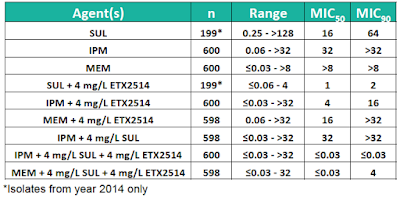 |
| Table 2: Activity spectrum of ETX2514. Source |
A follow up of this study was just presented at ID week. The MICs of nearly 600 isolates of A. baumannii are shown in Table 2. Most interestingly a triple combination of Imipenem or Meropenem/Sulbactam/ETX2514 brought the MIC90 to less than 0.03 mg/L. Microscopic studies showed that A baumannii became rounded and enlarged in the presence of ETX2514 further confirming the activity against PBP (See Photo 1). Remember, PBP is essential for cell wall and structure maintenance.
 |
| Photo 1: Effects of ETX2514 on A baumanii cell structure. Source |
Traditionally, beta lactamase inhibitors have a limited range of a molecular class of β-lactamase that can be inhibited. But ETX2514 is designed to broadly specific and hence has an upper hand. So, will the strains that are resistant to ETX2514 automatically be resistant to a huge range of BL/BLI combination. Since this will be used when the bugs are already resistant to traditional BL/BLI combination does that matter?
To answer that question, we need to look at mutants. Several mutants of A baumanii strains have been recovered while studying ETX2514 activity. The frequency of resistance was 7.6 x 10-10. These strain have been sequenced by WGS. The resistance was mapped to residues S390T, S395F or F548C in PBP3 or to mutations in tRNA synthetase genes (aspS and gltX). The latter is associated with resistance to PBP2 inhibitors in E. coli. Purified mutant PBP3 proteins had reduced affinity for sulbactam and variable affinity for Imipenem and Meropenem.
Now put this whole thing in context. Sulbactam attacks PBP1 and 3 but not 2. There is evidence that ETX2514 attacks PBP2. So when everything combines together, the antimicrobial activity is good. Even in diverse cases since there is a difficulty in having all PBP1-3 in mutated form. So any beta lactam drug that doesn't work on PBP2, but does so with others is a good to go combination. An example would be aztreonam. The activity will not synergistically increase with β-lactamase such as mecillinam which specifically binds PBP2.
Now put this whole thing in context. Sulbactam attacks PBP1 and 3 but not 2. There is evidence that ETX2514 attacks PBP2. So when everything combines together, the antimicrobial activity is good. Even in diverse cases since there is a difficulty in having all PBP1-3 in mutated form. So any beta lactam drug that doesn't work on PBP2, but does so with others is a good to go combination. An example would be aztreonam. The activity will not synergistically increase with β-lactamase such as mecillinam which specifically binds PBP2.
This brings in another question as to how this fits into real world scenario. The study reported "BLAST analysis of 1,537 whole genome sequenced strains of A baumannii showed no variation in PBP3 at S390, S395 or V505. Nine strains were found to have a T511S substitution but no T511A variants were found. This suggests that pre-existing target-mediated resistance to sulbactam-ETX2514 is not a significant resistance mechanism in the clinical setting". But resistance will appear once the drug becomes widely used.
References
Penwell W, Shapiro A, Giacobbe R, Gu R, Gao N, Thresher J et al. Molecular Mechanisms of Sulbactam Antibacterial Activity and Resistance Determinants in Acinetobacter baumannii. Antimicrobial Agents and Chemotherapy. 2015;59(3):1680-1689.
Shapiro et al. ETX2514, a Novel, Rationally Designed Inhibitor of Class A, C and D b-lactamases, for the Treatment of Gram-negative Infections. Poster number LB-024. ASM Microbe; June 16-20, 2016.
Mcleod et al. Sulbactam combined with the Novel β-lactamase Inhibitor ETX2514 for the Treatment of Multidrug-resistant Acinetobacter baumannii Infections. Poster number 2246. ID week 2016. October 26- 30, 2016.
Shapiro et al. ETX2514, a Novel, Rationally Designed Inhibitor of Class A, C and D b-lactamases, for the Treatment of Gram-negative Infections. Poster number LB-024. ASM Microbe; June 16-20, 2016.
Mcleod et al. Sulbactam combined with the Novel β-lactamase Inhibitor ETX2514 for the Treatment of Multidrug-resistant Acinetobacter baumannii Infections. Poster number 2246. ID week 2016. October 26- 30, 2016.





Comments
Post a Comment